Can a herniated disc heal without surgery?
In this article, I take a deep dive into some of the current scientific literature to see if a herniated disc can heal on its own without surgery.
Contents
- How does a herniated disc cause pain?
- How does a disc herniate?
- Is a bulging disc the same as a disc herniation?
- How can a herniated disc get better on its own?
- How does the herniated disc reabsorb?
- Time is a major factor in the healing of herniated discs
- What are some tips for healing a herniated disc injury?
- When is it time to consider surgery for a herniated disc?
- What are some problems associated with back surgery?
Lower back pain and sciatica incur most time off work and disability of all medical conditions.
Lower back pain from disorders such as spondylosis and intervertebral disc protrusions/herniations were the 2nd highest ranking reason for hospitalized care in the working population (age 18–44) in the United States of America back in 2005.
Spinal surgeries have also been on the increase and surgeons now perform around 1.62 million instrumented spinal procedures every year, including surgeries that involve multiple procedures during the same visit.
However, surgery is not a guaranteed way out of pain and discomfort from a herniated disc and as you read on you will find out that surgery can also lead to the same problem reoccurring years later.
People should always explore conservative measures before going under the knife.
How does a herniated disc cause pain?
To further understand the mechanism of a herniated disc it is necessary to understand a little bit more about the physiology in that area.

The intervertebral disc is a cartilaginous structure that lies between each vertebra and it functions as a shock absorber and a spacer.
The outer portion of the disc is a tough fibrous structure known as the annulus fibrosis.
The annulus connects the two vertebrae together and helps to contain the more gelatinous center of the disc, the nucleus pulposus. This nucleus is made up mainly of water and helps to absorb shock through the spine
How does a disc herniate?
Discs herniate either by rupturing the outer layer of the disc (the annulus), or breaking the endplate off the vertebral body which then allows the soft gel-like center (the nucleus pulposus) to ooze out.
This gel can pinch or compress parts of the nerve root, causing pain such as sciatica.
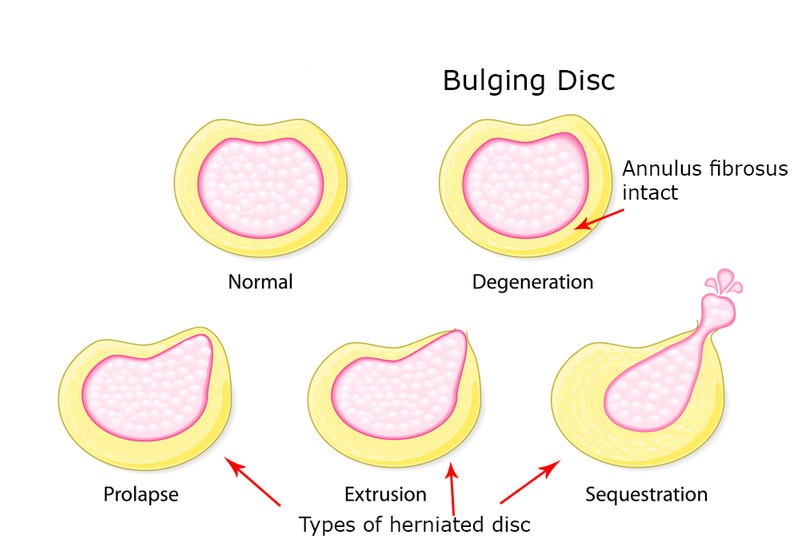
Is a bulging disc the same as a disc herniation?
You may hear these terms bandied about and think they are one and the same in fact many doctors will use them interchangeably but there is a definitive difference.
With a bulging disc the disc tissue has extended beyond the outer rim of the vertebral body but the outer annulus fibres remain intact and none of the inner jelly like nucleus pulposus has burst through the annulus fibres into the spinal canal.
A bulging disk is also called a prolapsed disc.
Compared with a bulging disk, a herniated disk is more likely to cause pain because it generally protrudes farther and is more likely to irritate nerve roots.
How can a herniated disc get better on its own?
There is a term which researchers call spontaneous disc reabsorption and it has been reported in numerous studies with the overall incidence being close to 70%. The disc material that was once protruding reabsorbs back into the disc space.
The time this can take varies from person to person but many researchers have found that it appears to happen anywhere from 6 to 12 months from the original diagnosis with some patients showing full reabsorption at 4 months.
What was interesting was that those with the greatest disc herniation (larger amount of discal material protruding) and even those with a sequestrated disk (where part of the nucleus pulposus has broken off) had quicker reabsorption than those with a smaller disc herniation.
I will touch on why this could be in the next section.
It should be remembered that in these studies the patients were following conservative therapies such as physiotherapy, NSAIDS, physical therapy and manual therapy.
This is why conservative treatment should always be your first choice.
How does the herniated disc reabsorb?
There are three main theories as to why the disc is able to reabsorb.
Gradual dehydration and shrinkage –
Your disc is 90% water and over time this water will be absorbed by the body, causing the herniated segment to shrink in size. As it shrinks it may no longer affect the nearby nerve and of course pain will be reduced.
Physiological mechanics –
While controversial, some will argue that tension applied by the Posterior longitudinal ligament leads to retraction of the herniated disc fragment back into the intervertebral disc space.
Imagine pushing against a rubber band and then the band pushes you back to where you started.
This is also the basis for movements like the McKenzie push up where some theorize that with extension exercises, the protruding portion of the disc can be moved inward and away from the spinal nerves.
An immune response by your body –
This is the most extensively studied theory with preclinical and clinical evidence to support it.
The herniated material is identified by the body as a foreign substance which leads to an immune and inflammatory response. This in turn leads to enzymatic degradation and macrophage phagocytosis which consequently results to disc reabsorption.
Depending on each individual’s clinical condition, it is possible that one specific mechanism or different combinations of the three may operate in spontaneous regression of the herniated disc tissue.
Time is a major factor in the healing of herniated discs
As I discussed earlier when we herniate a disc we also have tears in the annulus fibrosus.
The annulus fibrosus has a limited blood supply which is a necessary component for the body to repair itself and therefore these tears can take quite a long time to heal on their own.
The body needs to lay down a network of tough collagenous fibres which then promotes scarring and the area of the tear becomes plugged.
However, due to the limited blood and nature of that tissue this process can take up to 2 years to be complete.
In the early stages when the area is beginning to heal over the material is very weak and therefore prone to re-injury and of course another herniation.
What are some tips for healing a herniated disc injury?
Unload the disc –
You must unload the disc for a prolonged period of time in order for it to heal. Every time you exceed the fragile strength of the newly laid down scar tissue you may re-tear the healing “wound” and the process starts all over again.
You most likely will want to avoid forward flexion.
You can check out my video on avoiding spinal flexion before noon to find out about the benefits of this proven technique.
Try decompression stretches –
Decompression or traction has been used and studied by many practitioners as a way to help heal herniated discs and to reduce nerve pain issues such as sciatica.
It can help promote nutrient exchange and hydration of the discs and removal of inflammatory materials as well as increasing the intervertebral space and providing a suitable environment for the disc to reabsorb.
I used them extensively during my rehabilitation and still use them today to help keep my spine healthy.
Below is an instructional video where I teach how to perform a decompression stretch for the L5 S1 junction of the lumbar spine.
Rehabilitation –
Strengthening the muscles supporting your spine under the guidance of a trained therapist can assist in getting the muscles to take the load off the spine which will help unload the disc.
You want to ensure the exercise is progressive and that you are not “rushed” into things too quickly – you can check out my article on exercise and back pain here.
You also want to make sure you are learning to “brace” when you perform activities that will help to stabilize your spine and protect your discs. You can see my abdominal bracing video below.
Keep your hips mobile –
Keeping the hips and the musculature around the hips and pelvis limber ensures that we keep excess loads off of the lower back.
Very often when we have a back issue and the pain that comes with it we tend to tense up around the hip and pelvic region and those muscles go into spasm.
This only exacerbates the injury and the pain that comes with it so keeping this region supple and mobile is a good idea.
You can have a look at some of the stretches I recommend for the hip area in the YouTube video below.
Hydration –
Many of the tissues in the body are up to 90% water, (our spinal discs included) therefore it makes sense to ensure that we maintain our hydration.
If we are trying to stretch various tissues and muscles we want to ensure the tissue is hydrated and supple otherwise it will be like trying to stretch a piece of leather…it won’t stretch and may end up causing us pain.
Hydration is a factor in disc health and I have written about it previously in this post which I recommend you check out.
Time –
As I mentioned before the disc and annulus fibres take time to heal and we cannot expect success overnight.
We need to be patient and give the body time to heal itself and we need to put our bodies into the best position for that to happen.
When is it time to consider surgery for a herniated disc?
Obviously, there may be times where no amount of conservative treatment is helping so it may be time to think about surgery as an option when:
– Pain persists or is severely hampering your daily life
– Walking or standing is difficult
– Weakness and numbness progress and do not get any better with conservative treatments
– Bladder or bowel problems develop
However, even with surgery comes complications and all the principles of rehabilitating a disc injury I mentioned before hold true post-surgery.
What are some problems associated with back surgery?
Recurrent herniation –
If surgery has been prescribed for a herniated disc then in general a discectomy is successful at alleviating pain and enabling patients to return to normal daily activities. However, this procedure does not repair the annulus fibrosis and consequently as I mentioned with doing too much to soon it has been found that, 10% to 30% of patients experience symptomatic recurrent herniation.
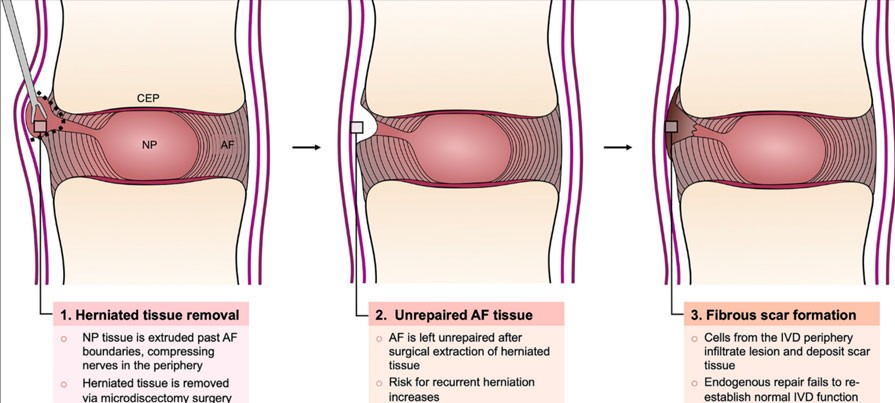
Increased risk of disc degeneration –
When you have surgery and they remove part of the protruding disc material you then have a reduction in the size/volume of the nucleus. This leads to less intervertebral disc pressure and disc height.
This can then alter the biomechanics of the disc increasing the risk of disc space collapse, abnormal facet loading and disc degeneration.
At the end of the day I would always recommend exhausting conservative treatments first before looking down the path of surgery. Herniated discs can indeed heal without surgical intervention but you have to lay the groundwork for that to happen.
Ultimately, you are aiming for a reduction in pain and a return to normal life and with the correctly implemented program this is within reach for the majority of people who suffer pain from herniated discs.
You first need to understand what has brought about the pain and why it hurts and then formulate a plan of attack to overcome that pain and heal your body.
If you or someone you know is still struggling with lower back/sciatica pain then please sign up for my weekly back pain recovery emails here.
If you would like more tips on preventing lower back pain then go over to my YouTube channel for even more educational content.

